This is an online E log book to discuss our patient's de-identificatied health data shared after taking her signed informed consent.
LONG CASE: 1601006099
A 65 yr old female, resident of narketpally, a house wife, came to the hospital with Chief complaints of
- Fever with chills since 8 days.
- Pain abdomen and loose stools since 6 days.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 8 days back, then she developed
- Fever, which was sudden in onset, low grade, associated with chills and rigors and relieved on medication.
- Pain in abdomen 6 days ago, sudden in onset, continuous, cramping/dull aching type, involving all quadrants and aggravated with food intake.
- Associated with 2-3 episodes/day of vomiting which was non bilious, non projectile and watery in consistency.
- Multiple episodes of loose stools 6 days back, which was watery and in large volume, no tenesmus, no mucous or blood in stools.
- History of burning micturition since 4 days, no froth/blood.
- No hematemesis/malena.
PAST HISTORY:
- She is a known case of diabetes since 10years
- History of hypertension since 10years
- No history of Tuberculosis, asthma, epilepsy, thyroid disorders, CAD, stroke.
DRUG HISTORY:
- Diabetes: Metformin 500mg
- Hypertension: Telmisartan 40mg
PERSONAL HISTORY:
- Diet mixed.
- Sleep disturbed due to frequent loose stools.
- Appetite decreased.
- Bowel movements- irregular
- Bladder- urgency and incontinence
- No known allergies
- No alcohol
- No smoking
FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Well oriented to time place and person. Moderately built & Well nourished.
- Pallor: present
- No Icterus, Koilonychia, Clubbing, Lymphadenopathy, Edema.
Vitals
- Temperature: afebrile
- BP: 110/80 mm hg
- Pulse: 92 bpm
- Respiratory rate: 20 cycles/min
- SpO2 96%
SYSTEMIC EXAMINATION:
Per Abdominal examination
Inspection:
- Generalised distention/fullness is seen.
- Shape: distended
- Flanks full
- Umbilicus inverted
- Movements with respiration: equal in all quadrants. Rises during inspiration and falls during expiration.
- No visible pulsations.
- Skin over abdomen: Multiple vertical stretch marks, horizontal scars.
Palpation:
- No local rise of temperature.
- Tenderness: diffuse.
- Liver, Gall bladder, Spleen impalpable.
Percussion:
- Shifting dullness: not present
- Fluid thrill: not present
Auscultation:
- Bowel sound heard
Other system examination
CVS
- S1 , S2 heard
- Apical impulse in 5th intercostal space lateral to mid clavicular line
- No murmurs
Respiratory system
- Bilateral air entry
- Normal vesicular breath sounds
- Bronchial breath sounds hear
- Trachea in the midline
CNS
- Gait normal
- Sensations normal
- Cranial nerve normal
- Reflexes preserved
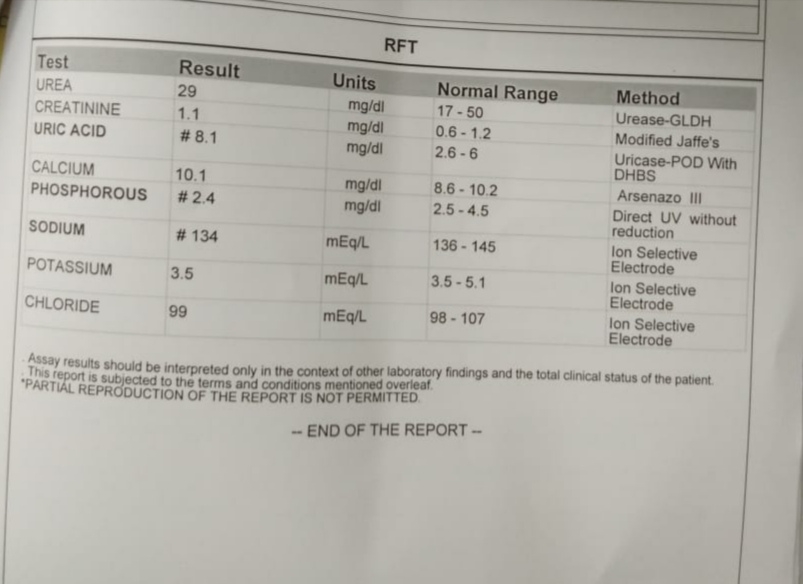
INVESTIGATIONS:
1. Stool examination & culture
2. Haemogram
3. Urine examination:
Increased pus cells in urine
4. Urine Protein/Creatinine ratio
6. Fasting blood sugar
7. Glycated Haemoglobin
PROBABLE DIAGNOSIS:
ACUTE GASTROENTERITIS
Treatment:
Tramadol inj
Ondansetron inj
Frusemide inj
Cefixime Tab








Comments
Post a Comment