MEDICINE CASE DISCUSSION
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
9th August, 2021
CASE SCENARIO
A 35 yr old female banker came to the casualty with complaints of fever since 4 days.
Headache since 2 days.
Nausea since 1 day.
Involuntary movements of right upper limb and lower limb since 2 hours.
HISTORY OF PRESENT ILLNESS
Patient was apparently alright 4 days ago then she had fever which was low grade, intermittent, relieves with medication, not associated with chills and rigors.
2 days ago she developed headache which was dull aching.
Today morning patient had weakness of Right UL and LL for which she took treatment at a local hospital. She left for work. After 1 hour while doing her bank work she suddenly had stiffness of her right upper limb and stiffness of neck and right side.
Later she developed involuntary movements of right UL and right LL.
Every episode lasts for 5 minutes.
No loss of consciousness. No involuntary micturition and defecation. No up rolling of eye ball.
On presentation to casuality she had 1 episode of involuntary movements of Right UL and LL.
HISTORY OF PAST ILLNESS:
No h/o diabetes, HTN, trauma, pregnancy, Asthma, TB and epilepsy
PERSONAL HISTORY
Appetite- decreased
Sleep- reduced
Bowel and bladder movements- normal and regular
Addictions- none
FAMILY HISTORY
Not significant
GENERAL EXAMINATION
Patient is conscious, coherent, co-operative.
Pallor+
No icterus, clubbing, lymphadenopathy, edema, pallor, cyanosis, kolionychia
VITALS
Temperature- Afebrile
Pulse rate- 74 bpm
BP-120/80 mmHg
SPO2 at room air- 99% at RA
GRBS- 119 mg%
SYSTEMIC EXAMINATION
CVS :
S1S2 HEARD
no thrills no murmurs
RS: B/L AE +
ABDOMEN:
Soft
Non distended
Diffuse tenderness absent
Guarding and rigidity absent
CNS
Right Left
Tone UL normal normal
LL normal normal
Power UL 3/5 5/5
LL 5/5 5/5
Reflexes
B- + +
T- + +
S- + +
K- + +
A- + +
P- flexed flexed
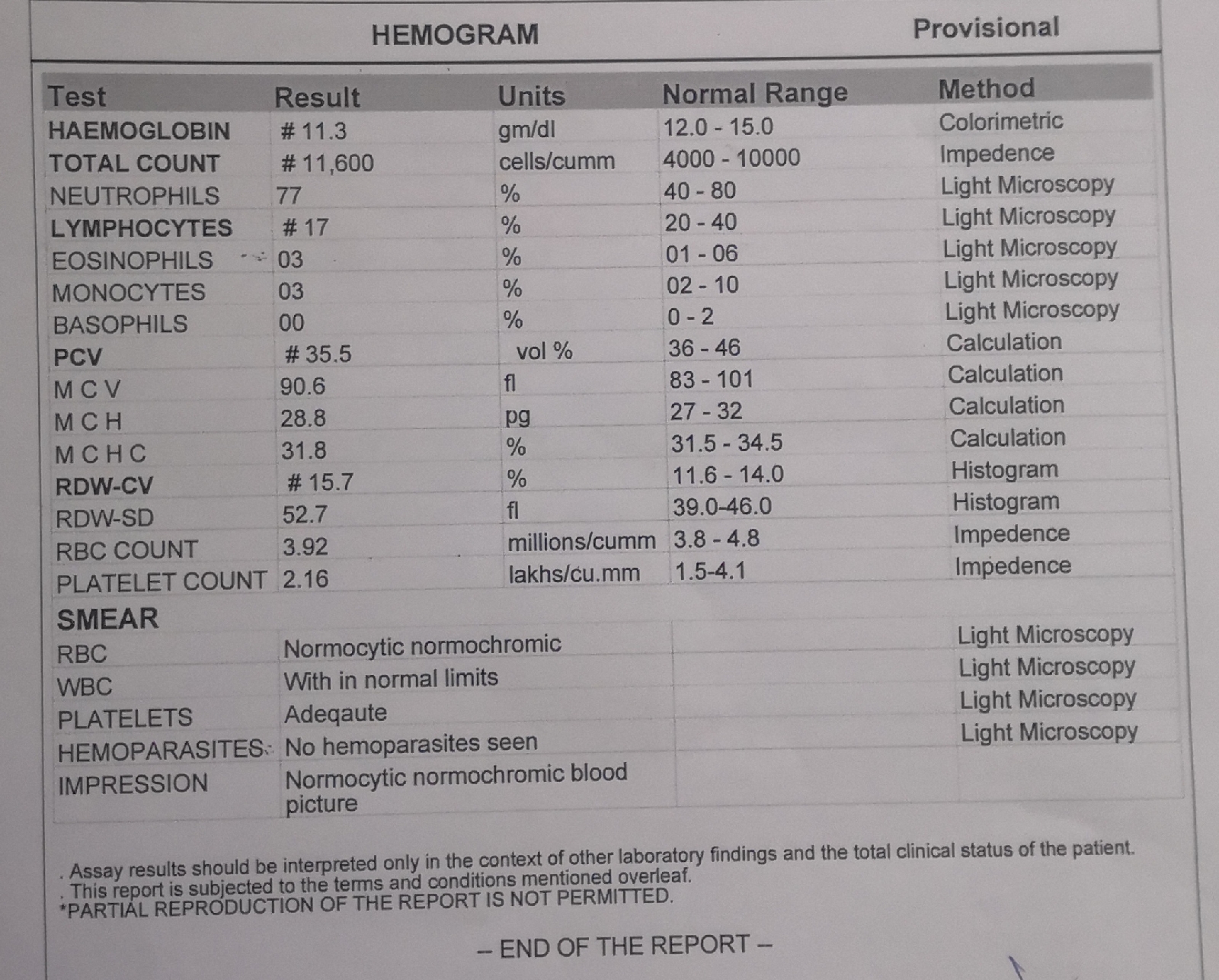
INVESTIGATIONS:
1. EEG
5. RBS
DIAGNOSIS: Cortical sinus thrombosis
TREATMENT:
Day one:
Inj. LEVIPIL 1gm/IV/BD
Inj. OPTINEURON 1 amp in 100ml NS/IV/OD
Inj. LORAZEPAM 2cc/IV/SOS
Tab. PCM 650 mg PO/TID
Inj. ZOFER IV/SOS
Inj. MANNITOL 100ml IV/TID
Temp charting 4th hrly
Day Two:
9th August, 2021 at 5:00pm there was an episode of GCTS
Inj. CLEXANE 40 mg x S/C stat given
COURSE IN THE HOSPITAL:
35 yr old female came to the casuality with c/o involuntary movements of right upper limb and lower limb since 2 hours. Additionally patient had h/o fever, headache and nausea. The patient was treated conservatively. On day two there was an episode of GCTS and Inj. CLEXANE 40 mg x S/C stat given. The patient wished to be shifted to another hospital and was discharged at request.




Comments
Post a Comment